Intermittent fasting can be an effective way of losing weight and helping you manage type 2 diabetes. Many members of our community are now free of diabetes medications, or have seen significant improvements in their condition.
How does it work? Fasting will help you lose weight, and lowers insulin resistance. This means it tackles the root cause of type 2 diabetes.
A word of warning: if you need insulin to control your diabetes you should not do intermittent fasting unless you have discussed your proposed fasting plan with your doctor – and unless you are very well trained in adjusting your insulin doses (for example by the DAPHNE programme)
What should I know about fasting with type 2 diabetes?
Start slowly
If you have type 2 diabetes you may find the first fasts particularly difficult as your high circulating insulin levels will make it hard for your body to switch into fat burning. Thus, it may be wise to start fasting gently by allowing yourself more calories in a day, or by only doing short fasts to begin with. As your body adapts to fasting, you can lengthen your fasts.
Experiment with different methods of fasting
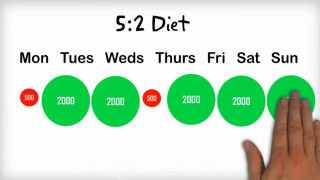
You may need to experiment with different methods of intermittent fasting to see which works best for you. Different people respond differently to fasting (and differently to different forms of fasting).
For example, many members of our community with type 2 diabetes tell us that a daily eating window approach works better for them than 5:2, as it combines weight loss with relatively stable blood glucose levels.
Learn more about eating windows and different ways of intermittent fasting
Limit your carbohydrate intake
To help keep your blood glucose under control you should limit all carbohydrates on both fast days and non-fast days. It is best to aim to keep your net carbohydrate intake below 100g per day, and these should come from foods with a low glycaemic index and glycaemic load.
In the past, you may have been told that you should eat plenty of complex carbohydrates for your diabetes. Unfortunately, science has now shown that this is bad advice. Eating carbohydrates increases your blood glucose, creating a need for insulin – and type 2 diabetes develops when your body is not creating enough insulin to cope. In short, eating carbs puts more pressure on your already-overloaded system.
Find recipe ideas for low carbohydrate meals and snacks.
Learn more about the metabolism of carbohydrates.
To learn more about the scientific evidence for low carb eating with type 2 diabetes, see the section below on ‘More information for the scientifically inclined.’
Go low-carb when you break your fast
It is especially important to choose lower carbohydrate foods as the first thing you eat when you break a fast. This might be your daily breakfast, or the first food you eat after a fast day.
In the mornings, you may find that your blood glucose tends to be higher (the ‘dawn phenomenon’) due to sugar production by the liver overnight. In this case, a small low-carbohydrate snack, such as a handful of nuts can help to turn off the release of sugar by the liver. Some people find that the morning rise in blood glucose is worse if the previous day has been one in which they ate a lot of carbohydrate.
It is also possible that your body is slower than normal to respond to glucose from your food immediately after a fast day. This might result in a higher peak of blood glucose than normal. To keep this peak to a minimum it is wise to choose lower GI foods – which generally means lower carb foods.
Be ready to adjust the dose of medications
The first adjustment you need to make to your medications will probably be on fast days. Your reduced food intake when you are fasting will lead to lower blood glucose levels and hence to a need to adjust your medication. (Note: monitor blood glucose regularly and remember that metformin doses do not need adjustment: see below)
After you have had some success and lost weight you may also find that you will need to adjust your medication on non-fast days. Again, you need to monitor blood glucose carefully so as to adjust your doses appropriately.
FastDay has many members with type 2 diabetes who have found that they have been able to withdraw some or all of their diabetes medications permanently. We think this is great, and we are really proud of them!
Remember you should always monitor your blood glucose carefully and that if you wish to discontinue a medication you should always consult with your healthcare team before making changes. (Note: It is recommended that, if you are taking metformin, you continue to do so – and this should be the last of your medications to be dropped because it works to reduce insulin resistance and so is complementary to fasting and low carbohydrate eating.)
Hypoglycaemic episodes
Some diabetes drugs, especially the sulphonylureas (e.g., glipizide, gliclazide, glibenclamide, glyburide, glibornuride, gliquidone, glisoxepide, glyclopyramide and glimepiride) can cause hypoglycaemic episodes (low blood sugar) as your insulin sensitivity improves during a fast, because they stimulate too much insulin release from the pancreas than is needed once your insulin sensitivity has improved. If you experience a hypoglycaemic episode, do treat it as normal with some carbohydrate, but also try to reduce your dose of medications rather than increase the carbohydrate content of your food on fasting days.
Exercise
Adding exercise to your day, particularly while you are still fasting, will further help to control your blood sugar and to reverse your diabetes. This is because exercise, like low carbohydrate eating and intermittent fasting, improves insulin sensitivity.
Learn about exercise and fasting
To improve your type 2 diabetes we recommend you should do all three of:
1. Intermittent fasting
2. Lower carb eating
3. Take some exercise
Intermittent fasting and type 2 diabetes research results
Studies have shown that:
-
Women with type 2 diabetes who fasted for 3 days showed lower blood glucose and enhanced insulin sensitivity.1
-
People with type 2 diabetes who extended their normal overnight fast from 12 to 18 hours showed a 23% fall in blood glucose concentrations between 12 and 18 hours of fasting.2
-
Men with type 2 diabetes who fasted for 24 hours showed a fall in blood glucose and insulin levels.3
-
Studies on fasting during the holy month of Ramadan have confirmed that fasting is safe for people with diabetes.4
Learn more about the health benefits of fasting and diabetes in particular.
More information for the scientifically inclined
Scientific evidence for the benefits of combining low carbohydrate eating with intermittent fasting
A Swedish study5 examined the effects of three different diets on blood glucose and insulin in 19 subjects with type 2 diabetes. The calorie content in all the diets was the same.
The first diet was a conventional low-fat diet (45–56% of energy from carbohydrates, which represents over 200g of carbohydrates per day); the second was an intermittent fasting regimen in which people skipped breakfast and then followed a Mediterranean diet with moderate carbohydrates (32–35% of energy, which represents around 150–175g of carbohydrates per day), they had a large lunch which had the same number of calories as breakfast and lunch combined in the other diets; the third was a low carbohydrate diet (16–24% of energy, which represents about 80-120g per day). All participants tried all three diets, one diet each day in randomized order. See the chart below.
The effects of diet on blood sugar levels throughout the day
Red line shows the low fat diet
Green line shows intermittent fasting
Blue line shows low carbohydrate diet
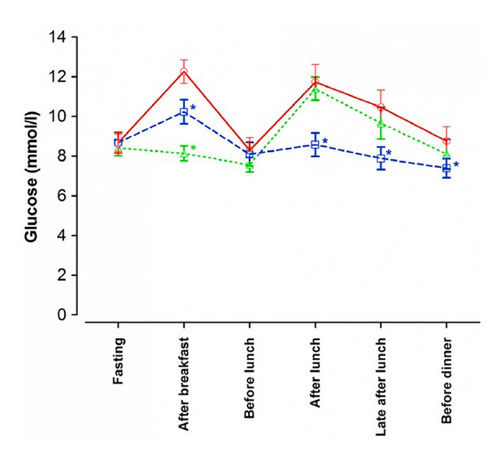
The low-fat diet (that most people with type 2 diabetes are still advised by their doctors to follow) actually produced the worst blood sugar levels throughout the day, with high peaks and overall higher levels of blood glucose than the other diets. The medium carbohydrate diet combined with skipping breakfast led to excellent blood sugar levels in the morning, and while the big lunch did cause a spike in blood sugar levels, these were no worse than those after the small lunch on the low-fat diet. The low carbohydrate diet gave much smaller peaks in blood sugar after breakfast and lunch resulting in the lowest average blood sugar levels throughout the day.
The changes in insulin levels showed a similar pattern as shown in the chart below (figure 2). With skipping breakfast on the intermittent fasting plus medium carbohydrate regimen, insulin levels were kept very low for an extended time, but it is important to note that the big lunch caused a large increase in insulin, showing the importance of breaking the fast with low carbohydrate food.
The changes in insulin levels throughout the day
Red line shows the low fat diet
Green line shows intermittent fasting
Blue line shows low carbohydrate diet
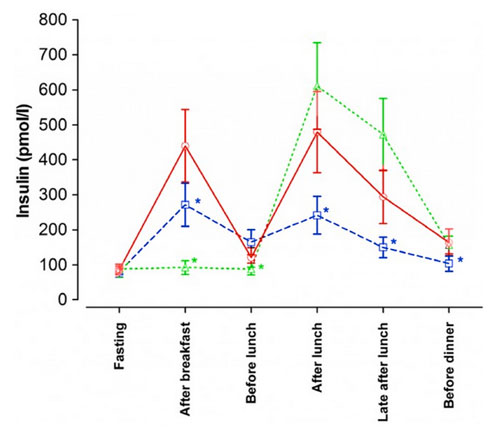
Unfortunately, the researchers did not examine what happens when intermittent fasting is combined with a low carbohydrate diet, but it is probable that one would gain the benefits of both.